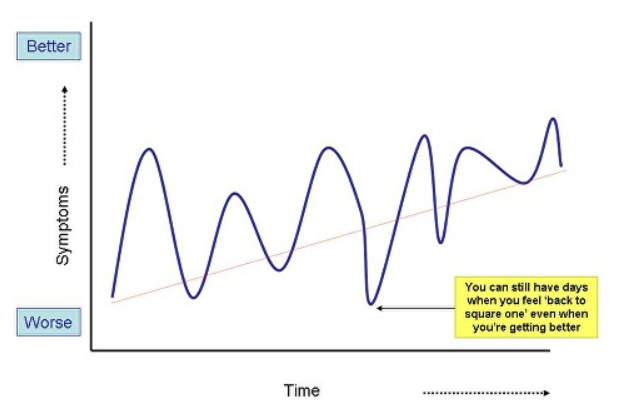
FND symptoms quite commonly relapse.
It’s one of the most crushing aspects of the condition that even when you think your symptoms have gone or are only in the background, then they may just creep up on you again, or, ‘bam’, suddenly appear on a Tuesday morning for no reason, even after many months or even years.
There are people with FND who do just recover and don’t relapse, so it’s not inevitable but it’s common enough that usually I like to have a conversation about this with people who have FND and have made a good recovery, so they are properly prepared – just in case.

So here are my top ten tips for dealing with relapses
This page was written with the help of colleagues including Glenn Nielsen at St Georges Hospital London who has led on physiotherapy rehabilitation for FND as well as Kate Holt, Mark Edwards, Alan Carson and Izzy Williams.


Ohjaamme sinut Edinburghin yliopiston lahjoitus-sivustolle. Lahjoituksia käytetään sivuston ylläpitoon ja toiminnallisten häiriöiden tutkimiseen.
