Dizziness is a common symptom in neurology and has lots of different causes – migraine, middle ear problems (vestibular disorders – like BPPV or labyrinthitis ) – and drug side effects.
Dizziness occurring as part of a functional disorder is also relatively common accounting for up to 20% of patients seen in a specialist dizziness clinic. When dizziness occurs as a functional disorder it is called
Other names for it include Visual Vertigo, Phobic Postural Vertigo, Functional Dizziness, Chronic Subjective Dizziness or Space and Motion Discomfort
PPPD has recently been defined by the World Health Organisation as
Lets look at a typical history of someone with PPPD.
Clara is a 24-year-old woman who has had persistent dizziness for the previous two years. She had an initial illness where everything was spinning really badly (vertigo) she felt sick and could hardly get out of bed for a week. The doctor made a diagnosis of viral labyrinthitis – this is a viral infection of the middle ear that causes dizziness and usually resolves in a week or two.
As she recovered her complaint of dizziness changed to a more non-specific feeling of dizziness that she found really hard to describe to people. It wasn’t the spinning sensation anymore. She said that she felt light-headed as if she was swaying and had a feeling of motion present mainly on standing and walking but also had noticed it when lying in bed at night.
Every now and then she felt ‘spaced out’ as if she was floating and people seemed far away which she found frightening.
She also found that she’d become really sensitive to objects moving in her environment when she was still. It was really difficult for her to use a computer or be in busy environments such as supermarkets. She found that she was quite often thinking about the possibility of falling. She had only ever fallen once but felt that she had experienced some ‘near misses’ at times.
The thought of being embarrassed and falling outside made her feel anxious and so she had tended to avoid busy places and going outside as much as possible.
Over time she had found that the dizziness had started to take over her life. Initially, she had become anxious about a possible sinister cause and had found herself looking up possible causes on the internet. She then saw doctors who had carried out detailed balance tests and she had a normal MRI scan of her brain.
Even when she became more confident that it wasn’t a sinister problem she found it very hard to cope with the symptoms. She developed symptoms of fatigue and poor concentration and had various periods of time off work. The whole thing was made worse by regular migraines during which her dizziness often got worse. She had occasional migraine.
She now felt at her wit’s end. What was causing this dizziness, why couldn’t anyone tell her what was wrong and how to get better?
Clara’s story is very typical. She started out with an episode of viral labyrinthitis that upset her balance system. Other people with PPPD start off with dizziness from migraine, or dizziness after a mild head injury.
These causes of dizziness all upset the normal processes that your brain uses to stop you feeling dizzy. Our brains are actually doing a lot of work all the time to stop us from feeling dizzy.
Our head, body and eyes can all move independently. Yet our brain is able to sort all this out to make sure that, for most of us, we don’t get abnormal sensations of movement.
It does this through an incredibly complex process using information from the middle ear, our feet and vision that neuroscientists are still figuring out the details of. It’s amazing it doesn’t go wrong more often!
If you want to read more about PPPD here is a link to an article written for neurologists about it
In PPPD what happens is that the normal ‘filters’ that the brain uses to suppress feelings of movement go wrong. Instead of the brain being able to balance everything up and give you a nice smooth feeling when you are moving, the person can feel a sense of movement that they shouldn’t.
After a while, because the person notices it a lot, they start to wonder what it is. Thinking about dizziness or worrying about it “turns up the volume knob” on the sensation. That makes it even stronger – and so the vicious circle begins. I’ve tried to show this in the picture below.
Like all functional disorders, this is not dizziness that is ‘all in the mind’. The person cant just switch it off. After a while, it becomes a constant intrusive sensation – a bit like a balance equivalent of tinnitus.
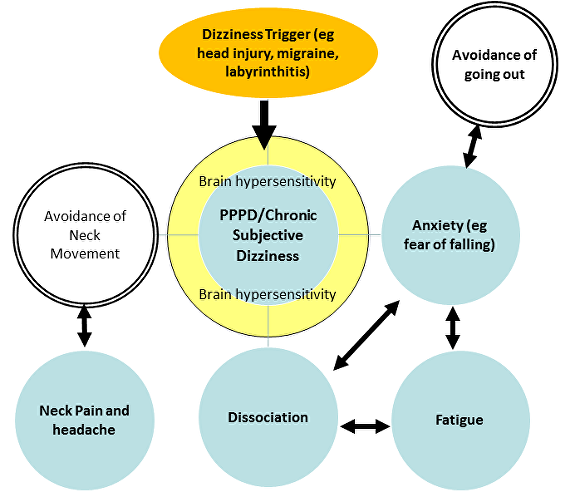
In PPPD one thing leads to another. Experiencing feelings of dizziness all the time understandably commonly causes anxiety. Anxiety about dizziness often revolves around concern about the cause, so-called health anxiety, although if no one tells you what’s wrong with you that is not really the same thing. Health Anxiety is when someone can’t stop worrying about a serious cause even though part of them knows that such fears are irrational.
Anxiety in PPPD may also be centred around concerns about falling or the consequences of falling such as embarrassment. Not everyone with PPPD has anxiety but it is common. The pathways for dizziness and anxiety in the brain turn out to be quite similar. Anxiety is really tiring for the brain. Fatigue is common in PPPD.

Often feelings of fatigue and dizziness merge with a ‘cotton wool’ feeling in the head which people sometimes refer to as ‘brain fog’. This is a feeling that merges between all of these symptoms as well as feelings of poor concentration.
People with PPPD become sensitive not only to their own movement but also to things moving around them. This has been called visual vertigo – although strictly speaking the dizziness of PPPD is not really vertigo. They can feel intense discomfort in places like supermarkets or on public transport or with patterned surfaces. This discomfort can lead to avoidance of those places and feelings of fear when asked to endure them.
Another consequence of PPPD may be Dissociation. This is described in more detail on its own page but is a feeling of being spaced out or zoned out. Sometimes people describe it as being disconnected or floating. Patients with PPPD may feel that they are walking on spongy ground sometimes or that their feet themselves feel spongy. There are other causes for this symptom but PPPD is one of them.
Neck movements may trigger feelings of dizziness in some people with PPPD (or indeed other balance problems). If you keep avoiding neck movements over a long time period then you may end up with a stiff painful neck or headaches. Worsening headache with dizziness only serves to make everything else worse.
PPPD is a problem with motion sensitivity. Problems with light and sound sensitivity or even nausea from smell sensitivity are more common in patients with PPPD. PPPD may be one component of chronic fatigue syndrome.
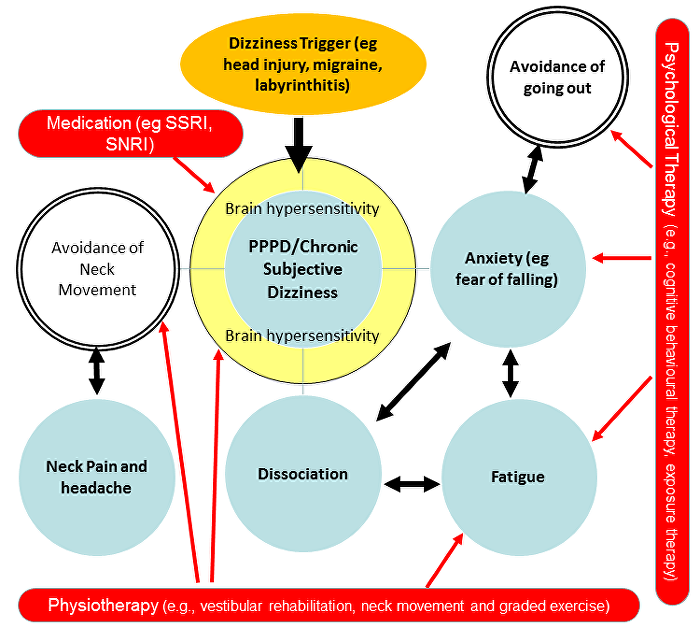
Specific treatment of PPPD takes time and there is no ‘quick fix’ but good recovery is certainly possible even after months or years of symptoms. Ingredients of treatment include
Matthew Whalley, a psychologist from Berkshire, UK and Debbie Cane, from the Manchester Centre for Audiology have published a really helpful guide to psychological treatment of PPPD. If you are a patient or a therapist wanting more direction this could be a very useful read for you.
Seeing a psychologist does not mean that your symptoms are ‘all in the mind’.
Have a look at this diagram again and think about things on it that could be changed by the treatments listed above.
Dizziness is a really difficult thing to describe to anyone, including doctors.
I’ve added this section to help patients talk more easily about their dizziness with doctors. Most patients with PPPD have a mixture of several types of dizziness and it can help to think about how to describe it
One simple way of dividing up symptoms of dizziness is into the following types
1. Lightheaded feeling that you’re about to faint (Presyncope) – if you have ever fainted you will know what this is! If you haven’t it may come as a new sensation to you. Typically this occurs when people are standing or if they have just stood up. It is a lightheaded feeling, sometimes with a rush of noise or fuzziness in the ears, a dimming of vision and often nausea. Doctors call this sensation presyncope. When someone actually passes out they call this syncope.
The causes of this include, standing up too quickly, and painful stimuli (like having blood taken or being at the dentist). It’s more likely to happen in hot places or if the person is eating. Men are especially prone to this when they are urinating while standing (especially in the middle of the night).
Faint feelings can also occur when people hyperventilate. This can happen during panic attacks but also as a more longstanding symptom in relation to breathing too fast or deeply. This is usually called hyperventilation.
Presyncope is not a functional symptom, but it’s worth knowing what it is as presyncope can trigger off other functional symptoms.
2. A feeling of movement (Vertigo) – This is when people describe a feeling of movement even when they are still. the movement may be a spinning rotating movement or a rocking movement like being on a boat. The medical term for this is vertigo.
Vertigo has lots of causes. The most common ones relate to problems with the structures in the ear which control balance. these are called semicircular canals. We have one set of semicircular canals in each ear. Most commonly bits of grit can get lodged in these and cause vertigo (this is called benign paroxysmal positional vertigo).
Migraine can also cause vertigo.
Vertigo is not a functional symptom, but like presyncope knowing what it is can be helpful. Some patients develop vertigo which then triggers off other functional symptoms
Vertigo is especially likely to induce anxiety in the sufferer.
Patients with vertigo often develop an aversion to moving their head. This is because head movement leads to vertigo. The trouble is, the more they avoid moving their head, the more likely it is that they will develop a stiff neck which in turn can lead to a sore head.
So people often develop a combination of neck pain, headache and dizziness which may have started out with vertigo but is still present even when the vertigo has gone. See below.
3. A spaced out feeling (Dissociation)– This may be dissociation, a feeling that you are distant or detached either from your environment or your body. This is described in detail on the page on dissociation on this website
Patients with dizziness may have one or more of these types of dizziness. Sometimes patients, especially those with fatigue describe even more vague symptoms like having a ‘foggy head’ or a ‘cotton wool head’.
4. A bodily feeling of unsteadiness (Dysequilibrium). This is a feeling sometimes compared to being on ice skates. It’s not so much a feeling of dizziness in the head. More a general feeling of unsteadiness as if something is wobbling around inside and that this could lead to a fall.


We will be re-directing you to the University of Edinburgh’s donate page, which enable donations in a secure manner on our behalf. We use donations for keeping the site running and further FND research.
