…During the attack you are losing control of your body. The aim of treatment is to find strategies to help you regain control. …
But in recent years there has been some progress in this area. This section is based on that research but also on the author’s own experience in trying to assist many hundreds of patients with these attacks to get better.
If you haven’t read them yet, have a look at these sections before you read on:
It’s really important to understand that these kinds of attacks are common, do not mean you are going mad or ‘losing it’, do not result in serious physical injury and are potentially reversible without medication.
It’s essential that you feel the doctor has looked into your case properly and come to the correct diagnosis.
If your doctor has referred you to a psychologist you may be wondering why. Read this section to help you understand this
The majority of patients with functional seizures have a warning before their attacks – not every time, and often it’s brief just lasting a few seconds.
Some patients have a warning but are unable to recall it after the attack. Sometimes a friend or relative will be aware of a warning even if the patient isn’t.
Some patients never have a warning and never become aware of it.
But learning to recognise the warning symptoms can be a key factor in learning to gain control of these attacks.
During the attack, you are losing control of your body. The aim of treatment is to find strategies to help you regain control.
A number of studies of patients with functional seizures have shown what kind of symptoms they can have in this warning phase. They showed that these symptoms are common just before many functional seizures:
These are all symptoms of ‘fight or flight’ when you have an adrenaline rush. They are also seen during panic attacks. They are symptoms of your nervous system being on “red alert”.
Similar studies have also shown that people with functional seizures were much more likely to develop a fear of going out alone, being somewhere where there are crowds, or where escape might be difficult. Often this happens because patients fear the embarrassment or fuss that might be caused by an attack.
Patients with functional seizures also sometimes feel concerned about the consequences of an attack. “Perhaps after one of these attacks, I might not come round?”, “Perhaps I might be left disabled, or ‘out of control’ in some way”.
Sometimes the functional seizure is your body’s way of “getting rid of” the horrible feelings you have during the warning phase. It’s not that you are deliberately blacking out but the blackout does at least bring the warning symptoms to an end and sometimes this is how a pattern of blackouts gets established.
Many people with functional seizures will say that at the point they are about to have the seizure, the sensations they are having are so unbearable that the seizure, although also horrible, does at least get rid of those feelings for a very short time. This can be a difficult thing to talk about but doing so can be a relief for some people.
Other people with functional seizures notice that there is a sense of something ‘building up’ in the hours or days before a seizure which is transiently ‘relieved’ by a seizure. They don’t want to have a seizure but they notice this pattern, which helps explain why it keeps happening.
So, you might ask, how does all this help?
If you can learn to recognise your warning symptoms, even if they only last a few seconds, you may, over time, be able to learn how to control them sufficiently to avert an attack and regain control of the situation.
What can you do to try to intervene when you get warning symptoms?
These may be some of the thoughts you are having –
“will I injure myself?”
“am I losing it?”
“will this be really embarrassing?”
“Is this epilepsy?”
“Might I die during an attack?”
There are answers to all these questions which are not as bad as you think
“will I injure myself?” ……………………………………..Possibly, bruises and bumps are common and occasionally patients may break a bone although that is rare. Doctors working in this area do not see patients with life-threatening injury. Part of you is aware during the attack, but you cannot remember it afterwards. This part of you appears to prevent really serious injury happening to you (or others, for example, a baby). this can’t be guaranteed and in particular, a very small number of patients appear to ‘self-harm’ during attacks without realising it.
“am I losing it?” ……………………………………………No, you are losing control temporarily but you are not going crazy or mad
“will this be really embarrassing?”…………………….Perhaps a bit, but is it really worth avoiding all the things you like to do because of that?
“Is this epilepsy?”………………………………………….No – if you’re not sure why not then ask your doctor
“Might I die during an attack?”………………………..No – this has never happened
The warning symptoms may ‘rush over you’ and it may be hard to focus on anything else but try to. In those few seconds before an attack, your thoughts may be overwhelmed by the physical sensations you are feeling.
If you can learn to focus on something else or distract yourself this may help. For example
These are the kinds of techniques that a psychologist can help you learn. They are also used to help people overcome panic attacks. Panic attacks and functional seizures are not one and the same thing. But they often have a lot in common, they’re a bit like cousins.
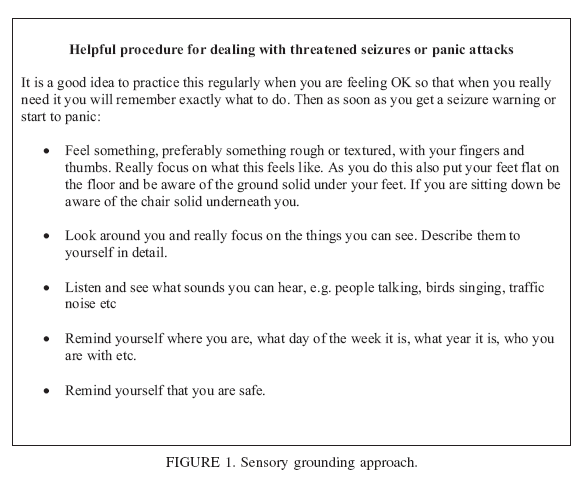
Another technique developed by researchers in Sheffield specifically for patients with dissociative seizures is called Sensory Grounding. (figure courtesy of Stephanie Howlett and Markus Reuber, University of Sheffield).
…Even though you can’t remember the attack, part of you is aware during the attack. …
… In a resting state, when you’re not distracted, your body is much more vulnerable to going into an attack….
There is more information about panic attacks on the website. Have a look at the page on anxiety and panic and the link to self-help material for panic attacks. Some of it might be relevant to you.
Here is a video made by Dr Courtney Raspin describing sensory grounding techniques
One problem can be that when you have an attack, people around about you become alarmed on your behalf. They may benefit from reading this website too. Even though you can’t remember the attack, part of you is aware during the attack. If people around you are upset this will make you worse.
People around you should: Stay calm, and supportive, make sure you have space around you, not put anything in your mouth, wait for the attack to settle and encourage you to get back up afterwards. You may even be able to carry on with what you were doing before, at work or at college for example.
Things that indicate you are making progress with these techniques include:
Patients with dissociative seizures are often really puzzled by the apparently random nature of their attacks.
Often they are completely random but sometimes they are less random than you might think. The commonest situations in which dissociative seizures occur are
When you are really feeling stressed, for example having an argument or rushing to get somewhere, your brain is often too distracted for the attack to take over. This is why dissociative seizures often don’t occur when people are really stressed about something else.
More treatment resources
More and more groups around the world are producing resources for people with functional seizures. Here are some of them. Some take a slightly different perspective to the one here but with many themes in common.
2. Dissociative Seizures – Right Decisions. A team based in Glasgow made this online app for people with functional seizures.
3. Taking control of your non-epileptic seizures. This factsheet was made by Markus Reuber and his FND research group in Sheffield .
4. Treatment manual for children and young people. This treatment manual produced by a team led by Dr Kasia Kozlowska in Sydney was made for health professionals working with children and young people with functional seizures.
This new treatment manual for functional seizures in young people is phenomenal – and free! Congrats to Kasia Kozlowska, Blanche Savage and all the authors. You can download it here – https://t.co/5VRNPDAELD pic.twitter.com/pa7M6jqp3L
— Jon Stone (@jonstoneneuro) January 17, 2023
Although its for health professionals, I find that patients and their families and friends may get a lot of insights into functional seizures from reading it. The book has been made free by Dr Kozlowska’s team at this link


We will be re-directing you to the University of Edinburgh’s donate page, which enable donations in a secure manner on our behalf. We use donations for keeping the site running and further FND research.
