- Links
- home-Symptoms
- Copyright and Terms and Conditions
- home-Symptoms
- home- ZASTRZEŻENIE
- home- ZASTRZEŻENIE
- home- ZASTRZEŻENIE
- home- ZASTRZEŻENIE
- home- ZASTRZEŻENIE
- {totalSearch} Results were found with `{searchKey}`
- Links
- home-DISCLAIMER
- FAQ
- How common is FND?
- Ive just been diagnosed and all I've been given is this website!
- If I already have FND but get new symptoms or a flare up, when should I seek a medical re-evaluation?
- What can I do to help myself if I'm waiting for treatment or not having treatment?
- Where can I find a healthcare professional interested in FND?
- COVID-19, the COVID-19 vaccine and FND. What do we know?
- I’ve heard people describing FND as Neuropsychiatric, doesn’t this mean that its psychiatric?
- Can people with FND have changes to the structure of their brain too?
- How reliable are the clinical Signs of FND?
- Isn't FND just a name for something when doctors don't know what it is?
- What makes clinicians confident that they are defining a discrete group of patients within the diagnosis of FND?
- Should people with functional seizures ever wear helmets to protect themselves from injury?
- Лечение
- Функциональная слабость конечностей
- Elementor #12975
- Functional (Dissociative) Seizures
- Chronic Headache
- Functional Tics
- Scan Negative Cauda Equina Syndrome
- Chronic Urinary Retention
- PPPD (Functional Dizziness)
- Functional Myoclonus
- Functional Cognitive Symptoms
- Functional Dystonia
- Drop Attacks
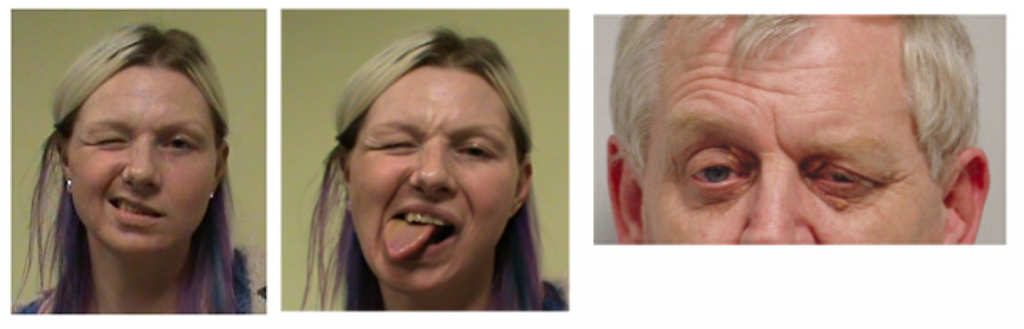
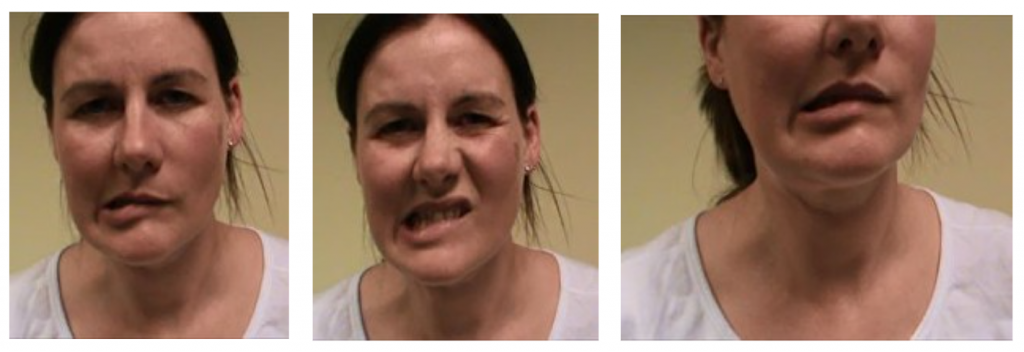
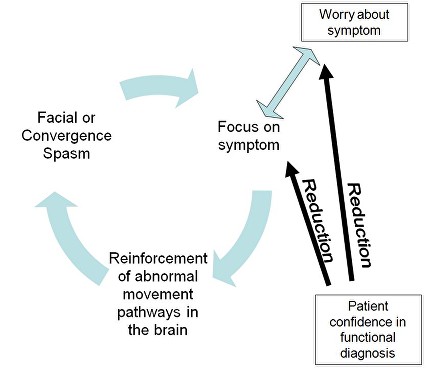
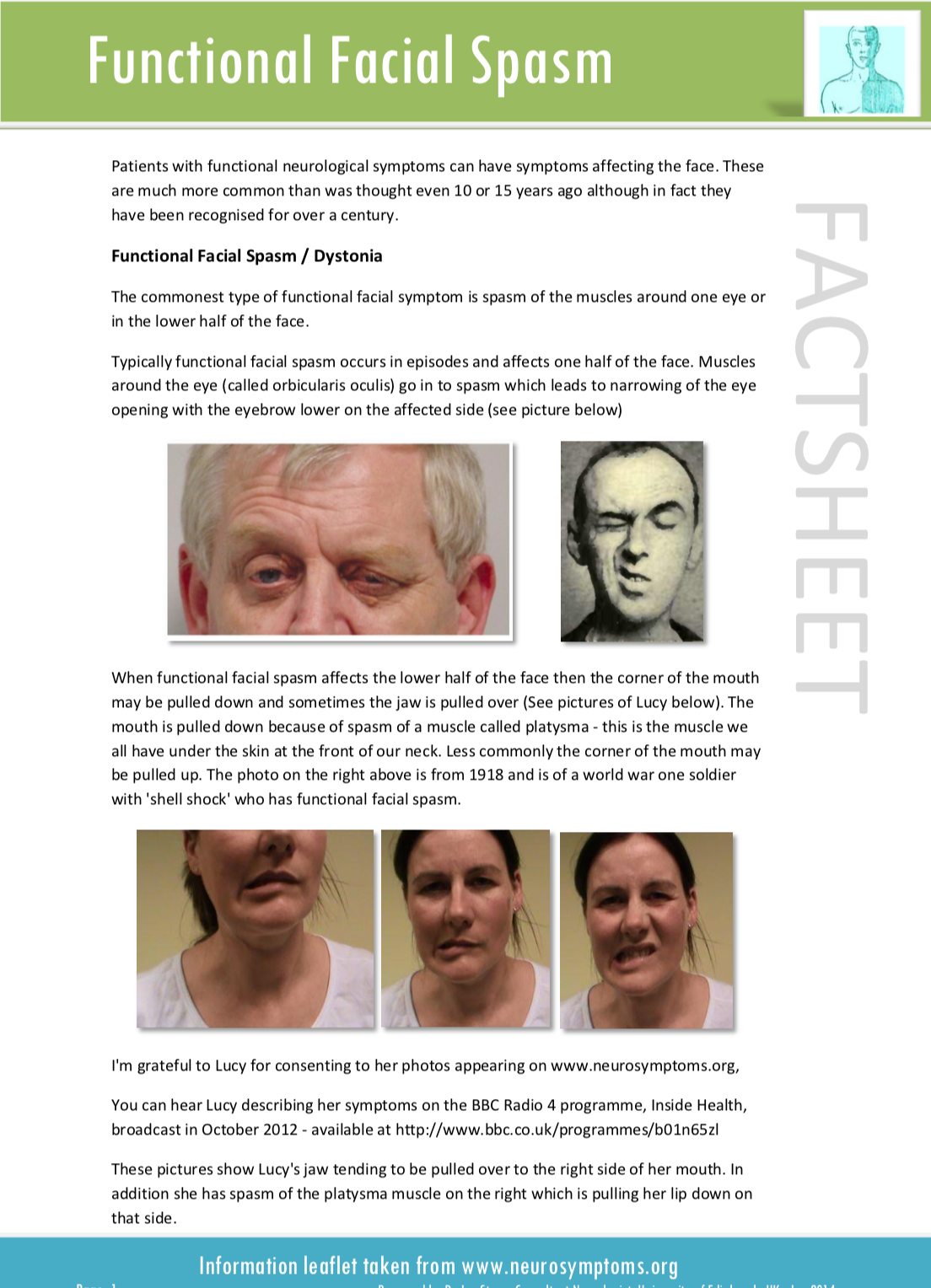
- Functional Facial Spasm
- Funksjonell bevegelsesforstyrrelse
- Функциональные спазмы в лице
- Функциональная дистония (патологические позы и спазмы)
- Функциональные спазмы в лице
- Функциональная дистония (патологические позы и спазмы)
- Функциональная слабость конечностей
- Лечение
- Лечение (обзор)
- Симптомы
- Functional Movement Disorders
- Боль
- Elementor #1150
- Elementor #1300
- Recommender
- Functional Dystonia
- FNL og andre funksjonelle lidelser
- Causes
- FND is not imagined
- Главная
- PPPD (Functional Dizziness)
- Domovská stránka
- Fact Sheets
- Mary’s Story
- Мне только что поставили диагноз, и все, что мне дали — это только этот сайт!
- Хроническая головная боль
- Функциональные тики
- Скан-негативный синдром конского хвоста
- Хроническая задержка мочи
- ПППГ (функциональное головокружение)
- Функциональный лицевой спазм
- Функциональный миоклонус
- Функциональные когнитивные симптомы
- Функциональная дистония
- Приступы падения
- Функциональный тремор
- Функциональные (диссоциативные) приступы
- Брошюры
- Авторские права
- ФНР и другие функциональные расстройства
- Неверный диагноз?
- Почему это случилось?
- Главная
- О нас
- Рекомендации
- Пациенты и профессиональные организации
- Главная – Лечение
- Главная – Причины
- home-overview
- home – About the Author
- Главная – видео
- Главная – обзор
- Главная – ОТКАЗ ОТ ОТВЕТСТВЕННОСТИ
- Главная — об Авторе
- Ссылки
- ФНР — выдумка?
- Причины
- home-DISCLAIMER
- Sobre los autores
- Home
- Home
- Home
- صفحه اصلی
- Elementor #593
- {totalSearch} Results were found with `{searchKey}`
- {totalSearch} Results were found with `{searchKey}`
- Ten Myths of FND
- ده افسانه از اختلال کارکرد ذهنی
- Visual Symptoms
- 症状
- فهم الاضطراب العصبي الوظيفي
- Elementor #939
- Häufige Zusatzsymptome
- How has it happened?
- Fact Sheets
- Functional Cognitive Symptoms
- Functional Limb Weakness
- Functional (Dissociative) Seizures
- Functional Tremor
- Drop Attacks
- Functional Dystonia
- Functional Myoclonus
- Functional Facial Spasm
- PPPD (Functional Dizziness)
- Chronic Urinary Retention
- Scan Negative Cauda Equina Syndrome
- Functional Tics
- Chronic Headache
- About Author-news page
- Home-page-content
- Recommender
- Causes
- Copyright and Terms and Conditions
- Feedback
- FND Links
- Media
- FND videos
- What is FND?
- How is FND Diagnosed?
- Can you have FND and another neurological condition?
- How is FND treated?
- What causes FND?
- FND video from Switzerland
- Three Families and FND
- Functional Neurological Disorder - an introduction
- FND Basics Q&A with FND Hope International
- 'dis-sociated'
- Edinburgh Fringe Event
- FND - on 'Insight' Australian TV
- FND - on Australian TV, 2020
- Georgia's Race Against FND
- How am I running when I can't walk?
- Kylee's story
- Mark Edwards
- Moments in the Mirror with Max
- My FND Recovery Story
- Jacquie’s FND story
- Other Media
- Neuroscience Films
- Pain Videos
- Living Proof – Stories of hope and recovery from Chronic Pain
- Tame the Beast
- Understanding Chronic Pain in 5 minutes
- Fibromyalgia - Living with Chronic Pain
- Sensitivity - to pain and abnormal sensations - how does it work in the brain?
- Neuroplasticity - You can rewire your brain!
- Calm the storm - an introduction to migraine
- Migraine - how does it work?
- The mysterious science of pain
- The mystery of Chronic Pain
- FND videos
- Home
- Links
- About
- Stories
- Symptoms
- Common Associated Symptoms
- FND Symptoms
- Functional Limb Weakness
- Functional (Dissociative) Seizures
- Functional Movement Disorders
- Functional Sensory Symptoms
- Functional Tremor
- Functional Cognitive Symptoms
- Functional Dystonia
- Functional Gait Disorder
- Functional Dizziness (PPPD)
- Functional Jerks and Twitches
- Functional Drop Attacks
- Functional Facial Symptoms
- Bladder symptoms and FND
- Functional Tics
- Visual Symptoms
- Functional Speech Swallowing Symptoms
- Treatment
- Understanding FND
- Investigations
- Physiotherapy / Exercise
- Occupational Therapy
- Psychological Therapy
- Speech and Language Therapy
- Medication
- Family and Work
- Treatment of Functional Seizures
- Treatment of Limb Weakness
- Treatment of Tremor / Spasms
- "I've tried everything, nothing helps"
- Managing Relapses
- Treatment Overview
- Videos
- War neuroses
- Shell Shock in Edinburgh